STARR Study Group, Meuffels, D. E., &...
New publication
STARR Study Group, Meuffels, D. E., &...
New publication
Arens T, Melick van N, van der Steen MC, Janssen...
Editor’s Pick Prof Stafano Zaffagnini Journal of Experimental Orthopaedics
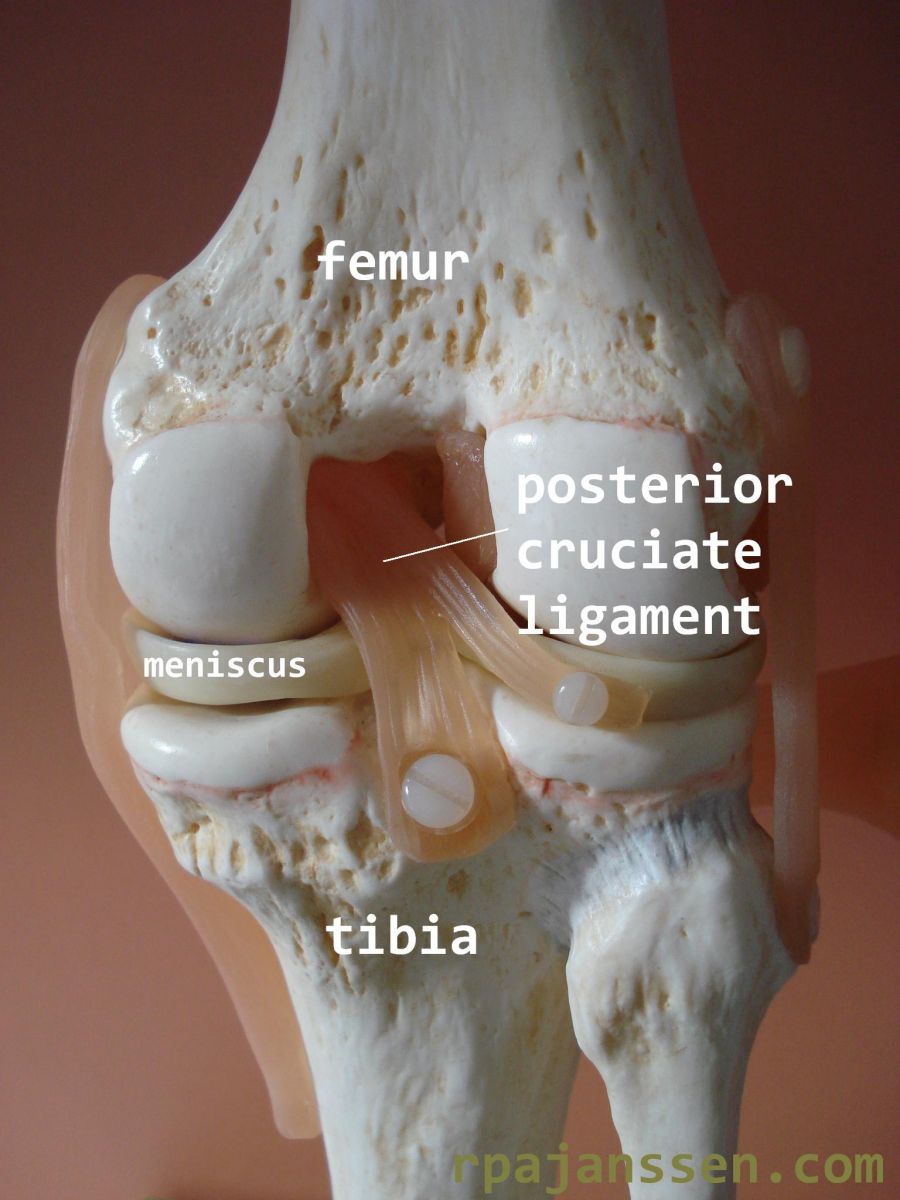
Posterior cruciate ligament
The posterior cruciate ligament is the strongest ligament in the knee. It forms the central pillar for stabilisation between the femur and tibia. The posterior cruciate ligament is situated in the center of the knee, behind the anterior cruciate ligament (see Information Cruciate ligaments-Anterior). Insertion sites of the posterior cruciate ligament are the inside of the medial femoral condyle and the posterior tibia. The main function of the posterior cruciate ligament is prevention of posterior luxation of the tibia.
Posterior cruciate ligament injury
A rupture or elongation of the posterior cruciate ligament is a serious knee injury. It is caused by traumatic posterior movement of the tibia relative to the femur or hyperextension of the knee. Common causes are motor vehicle accidents (dashboard trauma or motorcycle accidents). It may also occur in contact sports if a posterior oriented traumatic force is exerted on the tibia (goal keeper soccer, rugby, American football). Depending on the trauma direction and the position of the lower leg at time of impact, additional injuries may occur (posterolateral corner, collateral ligaments, meniscus and anterior cruciate ligament). Fractures may also occur. A posterior cruciate ligament lesion is common in knee dislocations. A knee dislocation occurs if more than 2 ligaments are injured in the kee. The posterior cruciate ligament does not often rupture; it usually elongates and continuity remains intact.
Diagnosis
The incidence of posterior cruciate ligament injury is low. For this reason, diagnosis is regularly missed in less experienced hands. Diagnosis is made based on patient history, physical examination, stress X-ray and sometimes MRI. Unfortunately, MRI is not always reliable in case of elongation of the ligament. It is essential to diagnose additional injuries for adequate treatment (especially posterolateral corner, meniscus, anterior cruciate ligament and vascular lesions). Numbness or paraethesia in lower leg and foot after trauma, suggest posterolateral corner injury. This occurs in 30% of patients. A posterior cruciate ligament injury is defined as acute if recognised within 2-3 weeks after injury. In these cases, conservative treatment is succesful if performed adequately (see Cases acute posterior cruciate ligament injury). After this time frame, the diagnosis is termed chronic and the ligament has lost its healing potential.
Symptoms
There are two type of symptoms after posterior cruciate ligament injury: giving way and patellofemoral pain (see Information Anterior knee pain). The giving way sensation occurs due to excessive posterior tibia movement. Patients often experience this on walking down stairs. Patellofemoral pain is due to posterior movement of the tibia; excessive pressure and larger lever moment on the patella lead to pain. .jpg)
Acute posterior cruciate ligament injury
Elongation of the posterior cruciate ligament may heal spontaneously if recognised and treated adequately within 2 weeks after the injury (see Cases Acute posterior cruciate ligament injury). Casting of the leg, with anteroposition of the tibia, is performed for 6 weeks. You will walk on crutches in this period and may partially weight-bear the injured leg. After these 6 weeks, rehabilitation is necessary to restore knee function and neuromuscular contol of the leg. Scientific research has demonstrated that conservative treatment is just as effective as surgery in acute injuries.
Chronic posterior cruciate ligament injury
A chronic posterior cruciate ligament injury no longer heals spontaneously. Surgical reconstruction of the posterior cruciate ligament is only indicated in case of giving way or serious patellofemoral pain. First, a brace is prescribed to determine if reconstruction is indicated for the symptoms presented. This brace is called PCL Jack or PCL Rebound brace. It is the only knee brace that gives dynamic and adequate support of the lower leg in posterior cruciate deficient knees. A special system of springs translates the tibia anteriorly in almost full knee range of motion. A surgical reconstruction is useful if complaints decrease in this brace. A posterior cruciate ligament reconstruction is more extensive in both surgery and rehabilitiation compared to an anterior cruciate ligament reconstruction. Associated posterolateral injuries should also be treated at time of surgery. This influences surgical time, however rehabilitation remains identical. 
Posterior cruciate ligament reconstruction
Surgery is perfomed through an arthroscopic approach. The deficient posterior cruciate ligament cannot be used and is removed. The posterior cruciate ligament is replaced by a autograft hamstring or an allograft. This tendon is fixed in bone tunnels in femur and tibia at the anatomic posterior cruciate ligament insertion sites. X-ray is used peroperatively to check adequate tunnel placement. The tendon is fixed by special fixation materials. These do not need removal in the future. After the surgery, the leg is placed in a long leg cast in extension. A drain remains in the knee for 12 hours to remove excess knee fluid. The drain is removed the day after surgery. Antibiotic prophylaxis is provided for 24 hours. Anti-thrombotic prophylaxis is prescribed for 6 weeks.
Rehabilitation
The physiotherapist will teach you to walk with 2 crutches on the first day after surgery. You may partially weight-bear the operated leg. Average hospital stay is 2-3 days. The knee remains fixed in extension in the cast till swelling decreases (usually 2-3 weeks, till the outpatient clinic appointment). Your own PCL Jack or PCL Rebound brace is then placed on the leg and should be worn for another 10 weeks. Advantage of the brace is the possibility to bend your knee. You may exercise knee flexion gradually while wearing the brace. Bracing should be 24 hours a day in order to allow the ligament to heal. The brace may be removed 3 months after surgery. The rehabilitation exercise program will then be intensified with your own physiotherapist. Total rehabilitation time is 6-12 months (see Protocol Cruciate ligaments-Posterior). Scientific research has demonstrated that some laxity remains on the reconstructed posterior cruciate ligament.
Complications
The complication rate is 1%: infection, vascular or nerve damage, compartment syndrome or venous thrombosis. The posterior cruciate ligament is situated in the posterior knee joint; a lesion to the nearby popliteal artery is a possible complication. For this reason, tunnel placement during surgery is controlled by X-ray. Knee surgeons agree internationally that this type of surgery should only be perfomed by experienced knee orthopedic surgeons in specialized knee centers. A vascular surgeon should be available in case of vascular complications. I make arrangements with the vascular surgeons at the Máxima Medical Center in all posterior cruciate ligament surgeries.